Why Are Open Standards Important In The Data Communications Industry?
Reading time: 14 minutes
COVID-19 has once again demonstrated the urgency of effective data commutation across health systems. To combat the illness, care providers, labs, insurance companies, public health agencies, and other players, demand a unified understanding and complete picture of the outbreak. And this can hardly be achieved without standards for recording and sharing clinical information.
Healthcare data standards existed long earlier the current pandemic. COVID-xix has simply emphasized their importance and ongoing problems. This article is besides short to cover all medical data norms but long enough to provide an overview of the well-nigh disquisitional ones. We'll also touch upon the standard evolution process and primary challenges related to standard adoption and usage.
Development of information standards
Data standards are created to ensure that all parties use the same linguistic communication and the aforementioned arroyo to sharing, storing, and interpreting information. In healthcare, standards brand upwardly the backbone of interoperability — or the ability of health systems to exchange medical data regardless of domain or software provider.
It normally takes 2 to 3 years to develop a new standard and ensure that it works properly. The entire cycle typically consists of the following steps.
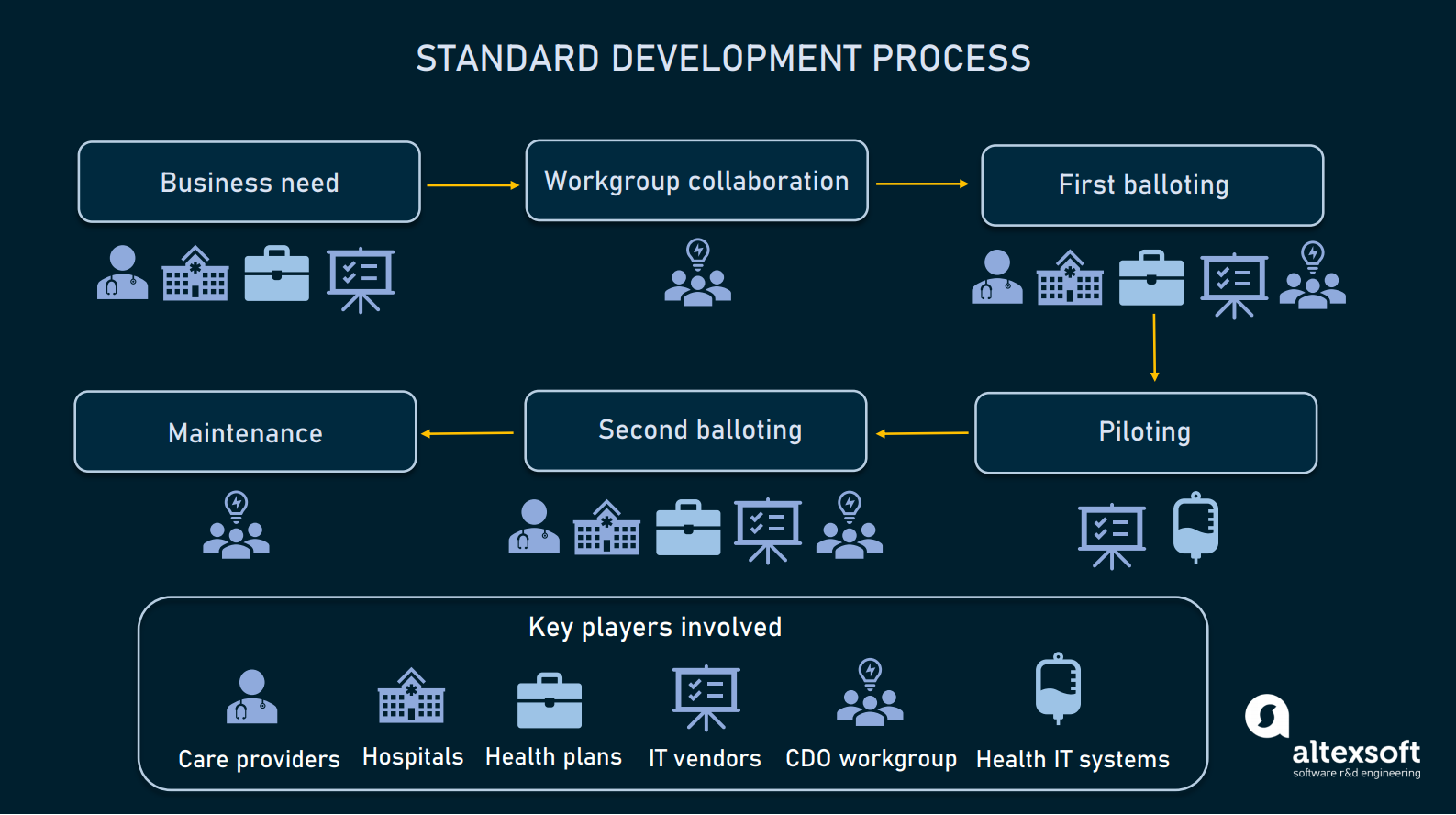
How healthcare standards are developed.
Identifying concern needs. Stakeholders (care providers, hospitals, wellness plans, or software vendors) place business needs and submit requirements for a standard to a standard development organisation or SDO.
Workgroup collaboration. The job to develop a standard is assigned to a workgroup, that may include clinicians, healthcare administrators, health information professionals, software developers, and experts in regulatory requirements. The workgroup designs the standard draft along with the implementation programme.
First balloting. Stakeholders give feedback on the typhoon and the workgroup incorporates it into the standards. Then, all participants vote for draft standards set for piloting.
Piloting. Healthcare systems and / or software vendors airplane pilot the draft version of standards and provide feedback.
Second balloting. The workgroup incorporates feedback from piloting and sends the typhoon for the second balloting. Upon receiving comments, the workgroup makes all necessary improvements. Finally, workgroup members and stakeholders vote to approve the typhoon as a normative standard for utilize.
Implementation and maintenance. The SDO implements standards, fixes issues, and collects feedback to make improvements.
As a rule, standard evolution is driven by non-turn a profit entities, and all experts engaged are volunteers who don't receive payment for this chore. The success of each standard heavily depends on the credibility of the SDO.
Key standard developers and types of standards
There are over 40 SDOs operating in the United states of america healthcare field and accredited by the American National Standards Plant (ANSI) or the International Organisation of Standardization (ISO). The list of the largest and most recognized SDOs include:
- HL7 — Health Level 7 International,
- NCDPD — National Quango for Prescription Drug Programs,
- IHTSDO — International Health Terminology Standards Development Organizations,
- DirectTrust Standards,
- CDISC — Clinical Data Interchange Standards Consortium.
Main standards created by SDOs and widely used across healthcare organizations fall into iv large groups:
- terminology standards,
- content standards,
- data exchange or transport standards, and
- privacy and security standards.
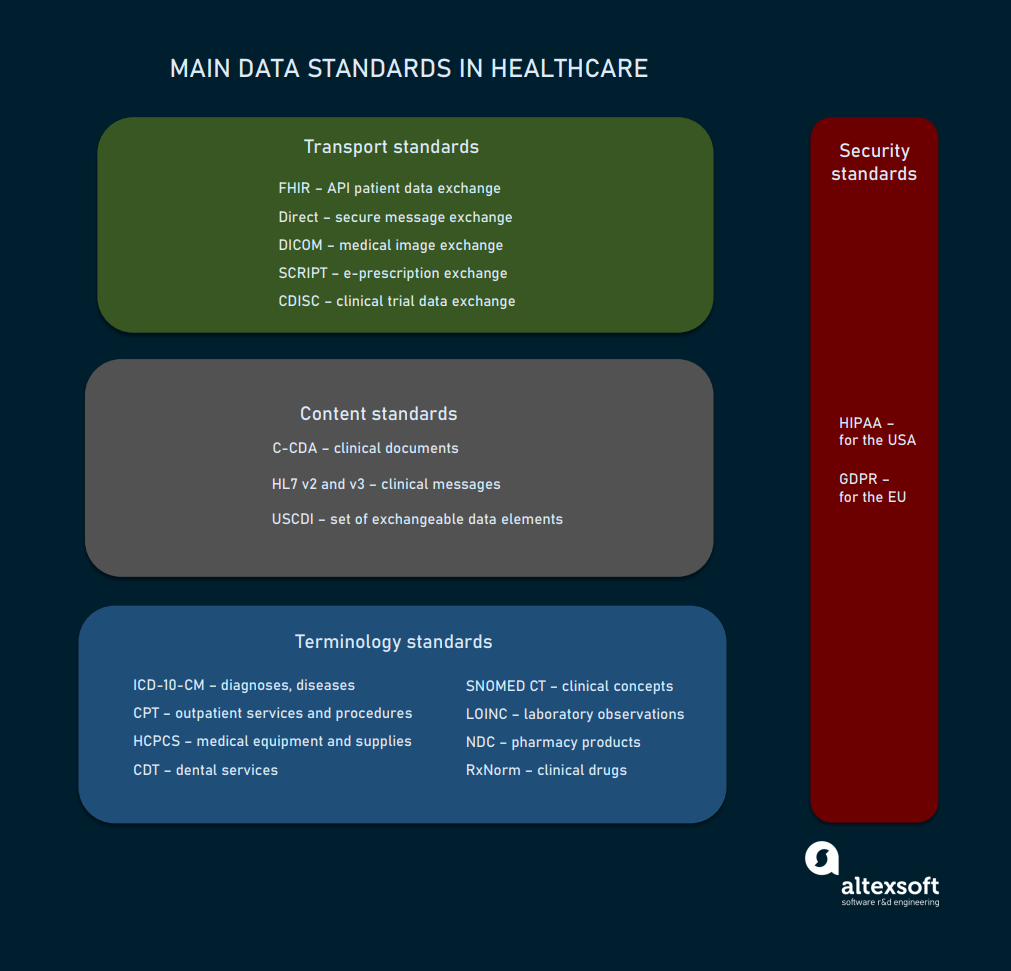
The list of key standards used in healthcare.
In the side by side sections we'll audit each grouping of standards separately to better sympathize their functions, level of adoption, and how they contribute to interoperability in healthcare.
Terminology standards
Wellness data may exist exchanged without terminology standards, but there's no guarantee that all parties volition be able to understand and employ information technology. Imagine that each organization calls the same disease or process by a dissimilar name. Or, vice versa, gives the same proper noun to different elements. The absence of a unified vocabulary leads to miscommunication, and in healthcare information technology can literally be a matter of life and expiry.
To avoid ambiguity and raise the clarity of content, healthcare systems rely on lawmaking sets and classification systems representing wellness concepts.
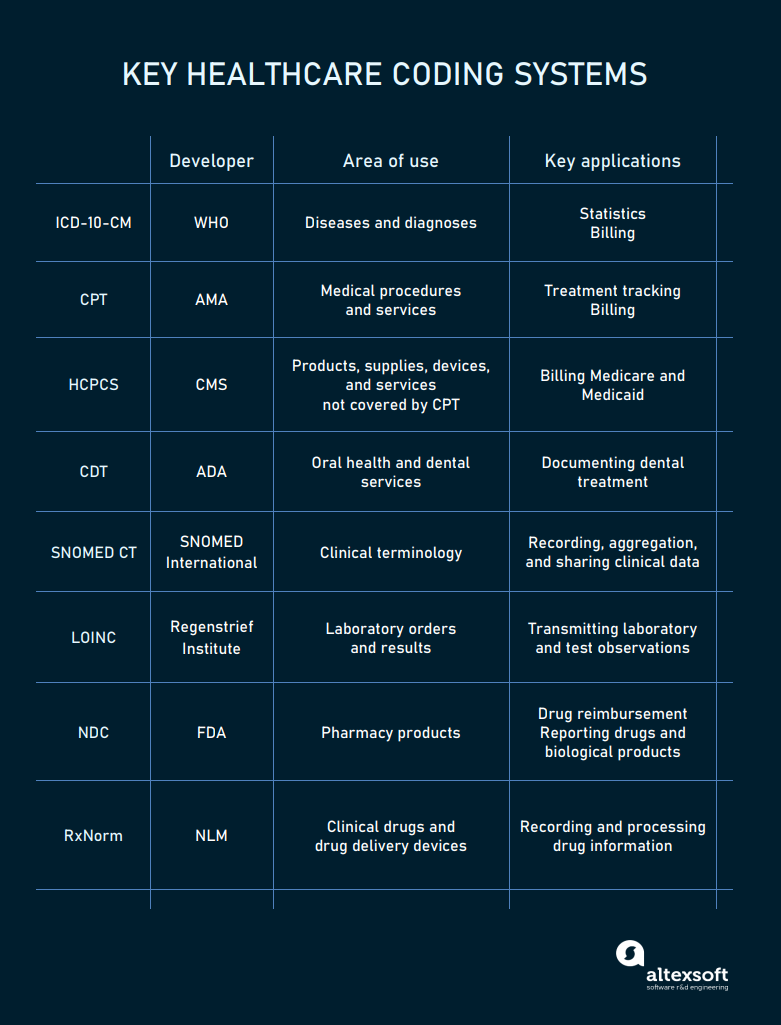
The main codes used in healthcare.
ICD-10-CM codes for diagnoses
The ICD-10, Clinical Modification (CM) is the United states version of the International Classification of Diseases, created and maintained by the World Health System (WHO). In the United States, ICD codes are revised by the Centers for Medicare and Medical Services (CMS) and the National Center for Health Statistics (NCHS).
In October 2020, the 10th revision of the code replaced the previous ICD-9-CM version. It contains over 500 updates, including new codes for vaping-related disorders and COVID-nineteen. The number of codes in the new version amounts to 68,000.
Hospitals mainly employ these codes for billing and reimbursement. Nationally and globally, the ICD serves as a universal tool to track morbidity and mortality statistics.
Under the ICD-ten-CM, every disease or health condition is assigned a unique code three to seven characters long.
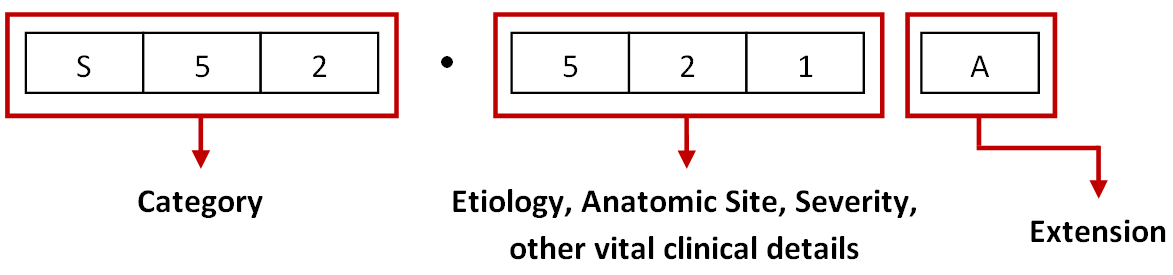
The ICD-x-CM code structure. Source: ViSolve
The first three elements represent a unique category, the second three digits describe etiology, anatomic site, severity, and other vital details, while the 7th character — or extension — specifies an episode of treat injuries, poisonings, and other conditions with external causes.
In 2022, the 11th revision of ICD codes will accept outcome, calculation two numbers for a more detailed diagnosis.
CPT codes for medical procedures
The Electric current Procedure Terminology or CPT is a code system maintained by the American Medical Clan (AMA). Information technology describes outpatient services and procedures for treatment tracking and billing purposes.
Each code contains v digits or four digits and one letter and is assigned to a particular procedure. Information technology is essential for getting payments from wellness plans. In a bill for reimbursement, a CPT number is paired with an ICD-10-CM code. If the service is not relevant to the diagnosis, the insurance company can reject the claim. Say, a doc is non supposed to send a patient with stomach ulcers for a chest Ten-ray.
Healthcare Common Procedure Coding System is an extended version of the CPT used to pecker Medicare, Medicaid, and other health plans. HCPCS (pronounced hick-picks) has two levels.
Level 1 duplicates CPT codes and identifies services and procedures ordered or delivered by physicians.
Level 2 contains codes with 1 letter followed by iv numbers. Supported by the CMS, it identifies services, supplies, and products not included in the CPT — like durable medical equipment, prosthetics, or drugs.
So, when are HCPCS codes used instead of CPT codes? If a service is described the same by both systems, and so the CPT is valid. If there is a demand to add more data, the HCPCS becomes operational.
CDT codes for dental treatment
Current Dental Terminology is developed and maintained past the American Dental Association (ADA) for electronic communication of dental services. Basically, CDT lawmaking covers oral health and plays the aforementioned role in dentistry equally CPT lawmaking in general healthcare.
A CDT code always starts with "D" and has a twin in the CPT code system as many health plans don't accept CDT codes for reimbursement.
SNOMED CT codes for clinical information
SNOMED CT stands for Systematized Nomenclature of Medicine – Clinical Terms and is owned by the IHTSDO. Recognized as a common language for medical terms in 50 countries, it enables intendance providers to accurately input patient data to the EHR system, aggregate information, and share it across health systems.
SNOMED CT encompasses far more concepts than ICD-10-CT. While the latter is limited to disease classification, the former covers symptoms, clinical findings, procedures, situations, substances, devices, and family history — in other words, almost any aspect related to healthcare commitment.
On the darker side, SNOMED CT is too granular to exist applied for reporting. Then, when information technology comes to billing, ICD-10-CT and CPT/HCPCS codes are used to capture a diagnosis and form of treatment and request reimbursement.
LOINC codes for lab orders and results
Logical Ascertainment Identifiers Names and Codes or LOINC is a fix of identifiers for laboratory tests and clinical observations. It was created by the Regenstrief Found with HL7 interoperability standards in listen. It covers the entire scope of existing lab tests and a broad range of clinical concepts and measurements.
Backed by the American Clinical Laboratory Association (ACLA) and the College of American Pathologists, LOINC codes are widely adopted by large commercial laboratories, hospitals, research institutions, and authorities agencies related to healthcare.
NDC codes for chemist's shop products
The National Drug Lawmaking (NDC) is a unique digit identifier for human medications in the The states. The coding system was created to facilitate processing of claims and drug data sharing. Currently, the codes are published on all drug packages and inserts.
The code contains 3 segments. The first five numbers represent a labeler (manufacturer, repackager, or distributor) and are assigned by the US Nutrient and Drug Assistants (FDA). The next 2 sections — 3-digit production and 2-digit package codes — are created by the labeler.
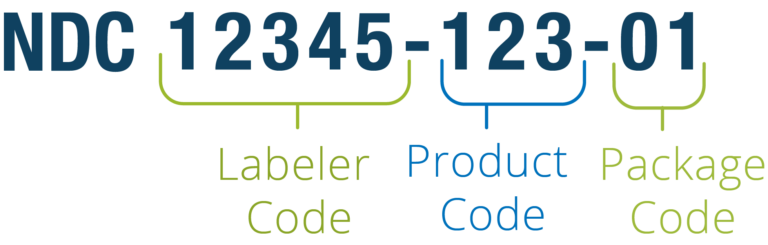
The NDC code structure. Source: Reed Tech
For example, if a manufacturer offers a drug in packages of two different sizes, each will have its own NDC. The aforementioned medication produced by two companies will as well be assigned 2 different identifiers. For billing, the code tin exist rearranged into an 11-digit string.
It may come as a surprise, but not every drug that has an NDC number was approved by the FDA.
RxNorm codes for clinical drugs
RxNorm is a catalog of all clinical drugs and drug commitment devices, available in the U.s.. Managed past the Us National Library of Medicine (NLM), it serves the purposes of interoperability, enabling clear advice between health systems, no matter the software they run.
The RxNorm code combines active ingredients, force, and dose form. And then, if these 3 attributes are identical, drug products will have the same identifier, regardless of brand or packaging. For example, Aspirin 325 Mg Oral Tablet has a single RxNorm ID — 211874. However, it can be marketed under dozens of different NDC codes — depending on manufacturer and package size.
Besides normalizing drug names, RxNorm links its codes to related brand-name and generic medications, as well equally to other commonly used drug vocabularies.
Content standards
Content or document standards dictate the structure of electronic documents and types of information they must incorporate. They ensure that medical data is properly organized and represented in a articulate and easy to understand form.
C-CDA for arranging clinical documents
Consolidated Clinical Document Architecture designed past HL7 is the principal framework for creating electronic clinical documents in the The states. It specifies how to structure medical records and how to encode data elements for substitution.
The standard allows for capturing, storing, accessing, displaying, and transmitting both structured and unstructured data, including texts, images, and sounds. Care providers tin can utilize different C-CDA document templates satisfying various information commutation scenarios — such as the following:
- the Consultation Notation template representing a response to the request of a practitioner for an stance from some other practitioner;
- the Continuity of Care Document (CCD) template to capture content that is critical to effectively continue intendance. This includes family history, allergies, data on recent infirmary encounters. The primary purpose of the CCD document is to exchange information on a patient existence transferred from one healthcare setting to another;
- the Belch Summary template to capture information about a patient's admission to a infirmary and the continuation of care after discharge; and
- the Diagnostic Imaging Report template to convey an interpretation of image data.
C-CDA documents contain a human-readable office that can exist displayed on a web browser, and a machine-readable Extensible Markup Language (XML) part intended for automated data processing.
HL7 version 2 and 3 for packaging data
A key divergence between an HL7 document (C-CDA) and an HL7 message is that the former is basically an electronic representation of a physical document while the latter is a packet of data sent from i arrangement to another.
U.s. healthcare relies primarily on version 2 and ii.ten messaging that is supported past every EHR system. Version 3 is widely adopted across the world, merely not in the United states.
Each HL7 message does its specific job identified by its name that contains 3 characters. The widely-used message types are
- VXU messages to ship vaccination history,
- ADT messages then ship demographic updates,
- QBP messages to asking immunization history, and
- RSP messages to return immunization history.

An example of an HL7 v2 message for sending demographic updates (ADT blazon). Source: Healthcare It Skills
Each bulletin is composed of several string-like segments, each starting with a 3-grapheme proper noun. Segments, in turn, incorporate fields that conduct data elements.
USCDI for specifying electronically available content
United states of america Core Data for Interoperability or USCDI is not a document or messaging standard, but a mandatory set of content pieces hospitals must share on a patient's request via APIs. The most granular parts of information — data elements — are aggregated in larger data classes similar Patient Demographics, Health Concerns, Medications, Procedures, and more.
In 2020, the Office of the National Coordinator for Healthcare IT (the ONC) finalized the commencement version of the USCDI standard. The second release will be bachelor for public feedback in 2021.
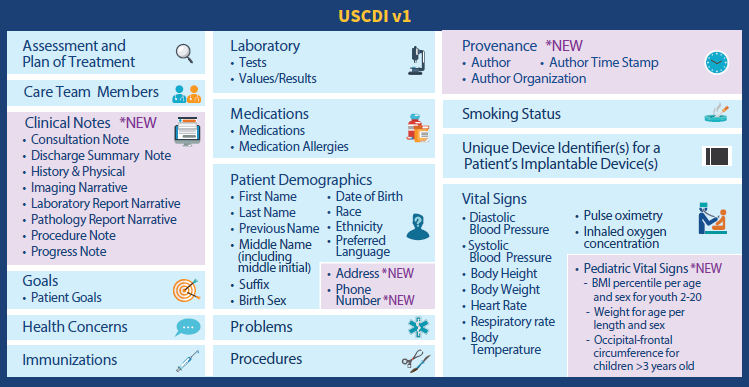
Electronically attainable data elements and classes specified by the 1st version of USCDI. Source: HIMSS Study
The next versions are expected to receive boosted data elements and classes. But besides specifying content to be exchanged, USCDI identifies terminology systems to be used. The listing of recommended code systems includes LOINC, SNOMED CT, and RxNorm.
Send standards
Send standards facilitate data exchange between different health systems. They define what formats, document compages, data elements, methods, and APIs to apply for achieving interoperability.
FHIR for patient access to medical records
Fast Healthcare Interoperability Resources or FHIR is an HL7 standard for transmitting healthcare information electronically. The Interoperability and Patient Access final dominion, issued by the CMS in 2020, requires all CMS-regulated payers to prefer version iv of FHIR. Unlike previous releases, the quaternary iteration is astern uniform so software providers can be certain that their products won't become obsolete one time a new FHIR version comes out.
The FHIR (pronounced "fire") standard provides a set of HTTP-based RESTful APIs, enabling healthcare platforms to communicate and share data represented in XML or JSON formats. FHIR supports mobile apps that patients may download from the Apple tree App Shop or Google Play to get their medical records and claims data.
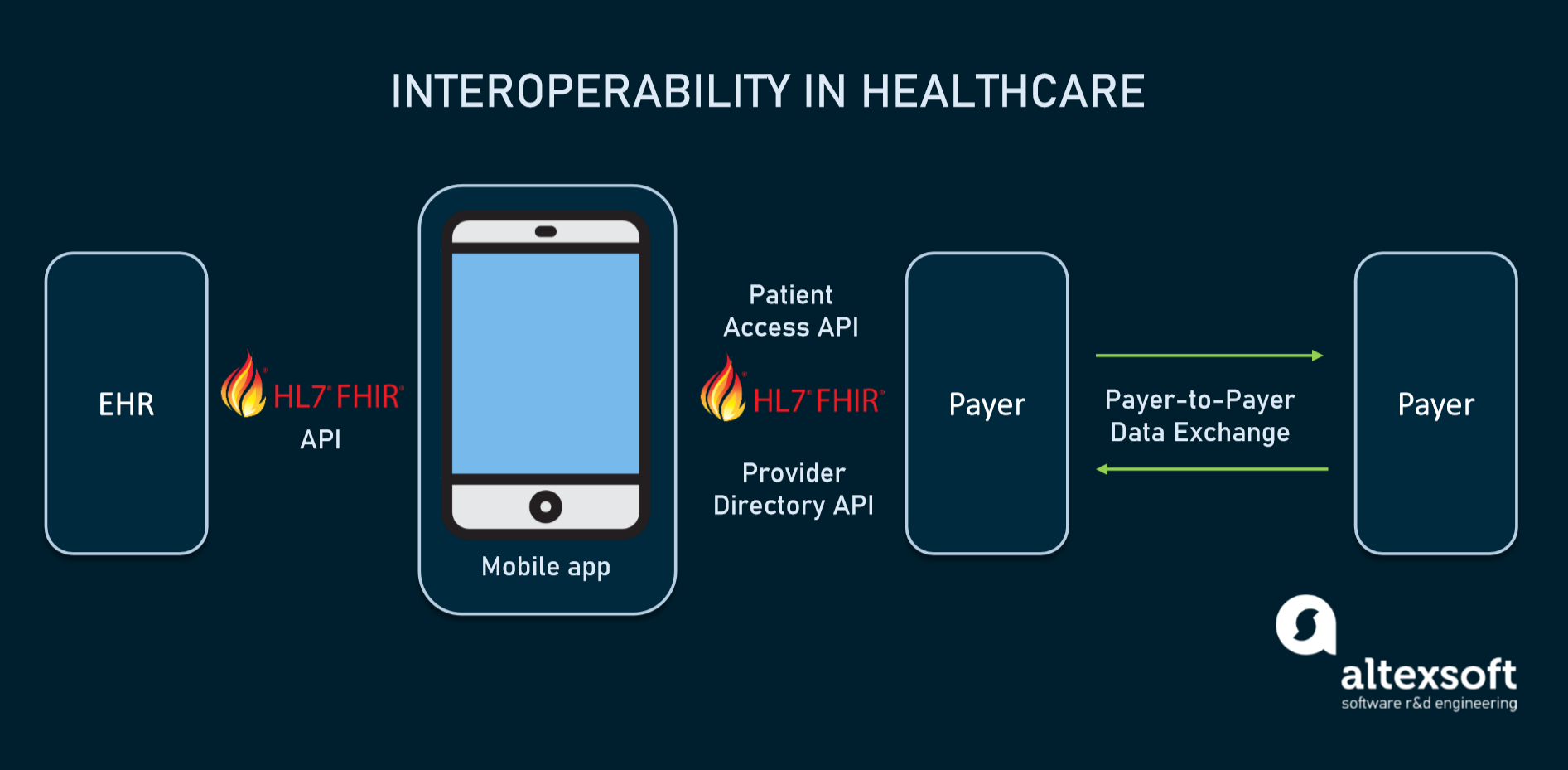
How interoperability in healthcare will piece of work using FHIR-based APIs.
The basic exchangeable data element of FHIR is chosen resources. Each resource is structured the aforementioned way and contains nearly the aforementioned amount of data. Depending on its type, it provides data on patient demographics, diagnoses, medications, allergies, care plans, family history, claims, etc. Altogether, they cover the entire healthcare workflow and tin be used separately or every bit a part of a broader document.
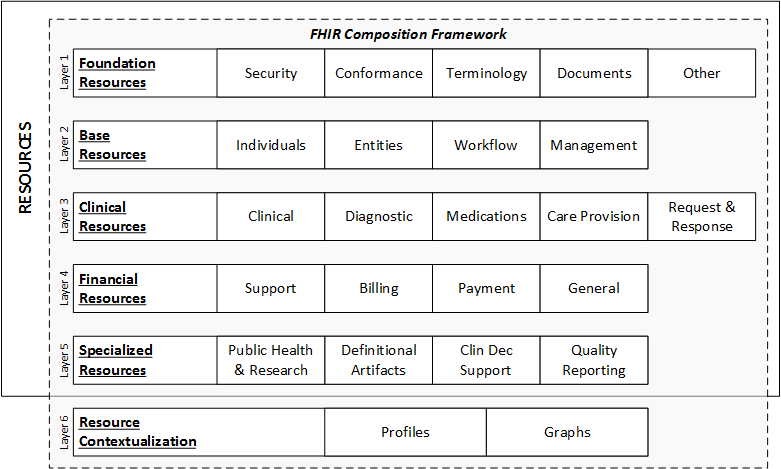
FHIR data layers and resources. Source: HL7 International
Each resource is assigned its unique ID and multiple stakeholders — health systems, insurers, patients, or software developers — tin retrieve the underlying data element via API.
Direct for exchanging personal health data
Direct maintained by DirectTrust is a well-known technical standard in utilise since 2010. It is widely adopted past EHR systems across the Us for the secure commutation of personal health data.
Direct messaging resembles electronic mail, merely with an added layer of security. Instead of SMPT (Simple Post Transfer Protocol) servers, it employs HISPs (Health Information Service Providers) to handle data exchange. HISPs provides encryption and digital signing of each message.
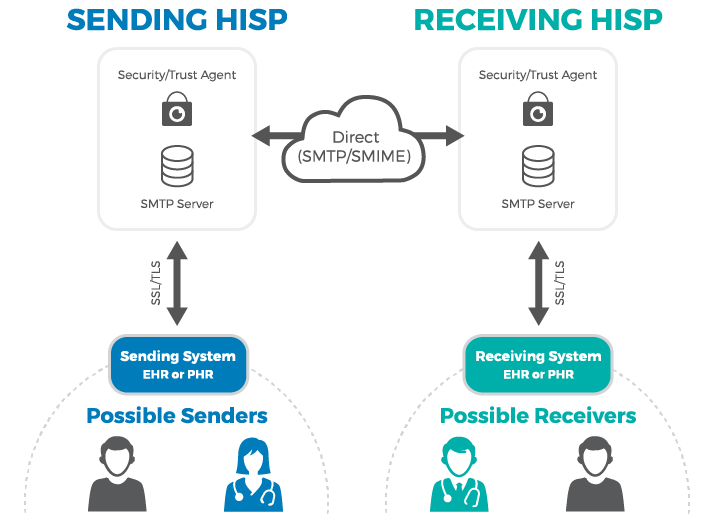
How Direct messaging via HISP works. Source: MedicaSoft
Currently, over 251,000 companies have DirectTrust addresses exchanging nigh 141 1000000 messages in 3 months. And this number will grow with the release of the Trusted Instant Messaging (TIM+) standard, which is already available for testing. When approved for use, it will allow all connected parties to exchange data in real-time.
DICOM for transmitting medical images
Digital Imaging and Communications in Medicine (DICOM) is an international advice protocol and file format for exchanging medical images and related data across hardware and software tools from dissimilar vendors. The tools in question include not only CT, MRI, and other scanners, simply also printers, image viewers, picture archiving and communication systems (PACSs), and radiologi information systems (RISs), to name a few.
Information technology's important to say that widely-used image file formats — JPEG, TIFF, or BNP — tell goose egg about the patient or epitome acquisition parameters. The standard addresses this problem, adding information necessary for diagnostic purposes. DICOM files with the .DCM extension contain a header with metadata and zero to several prototype pages.
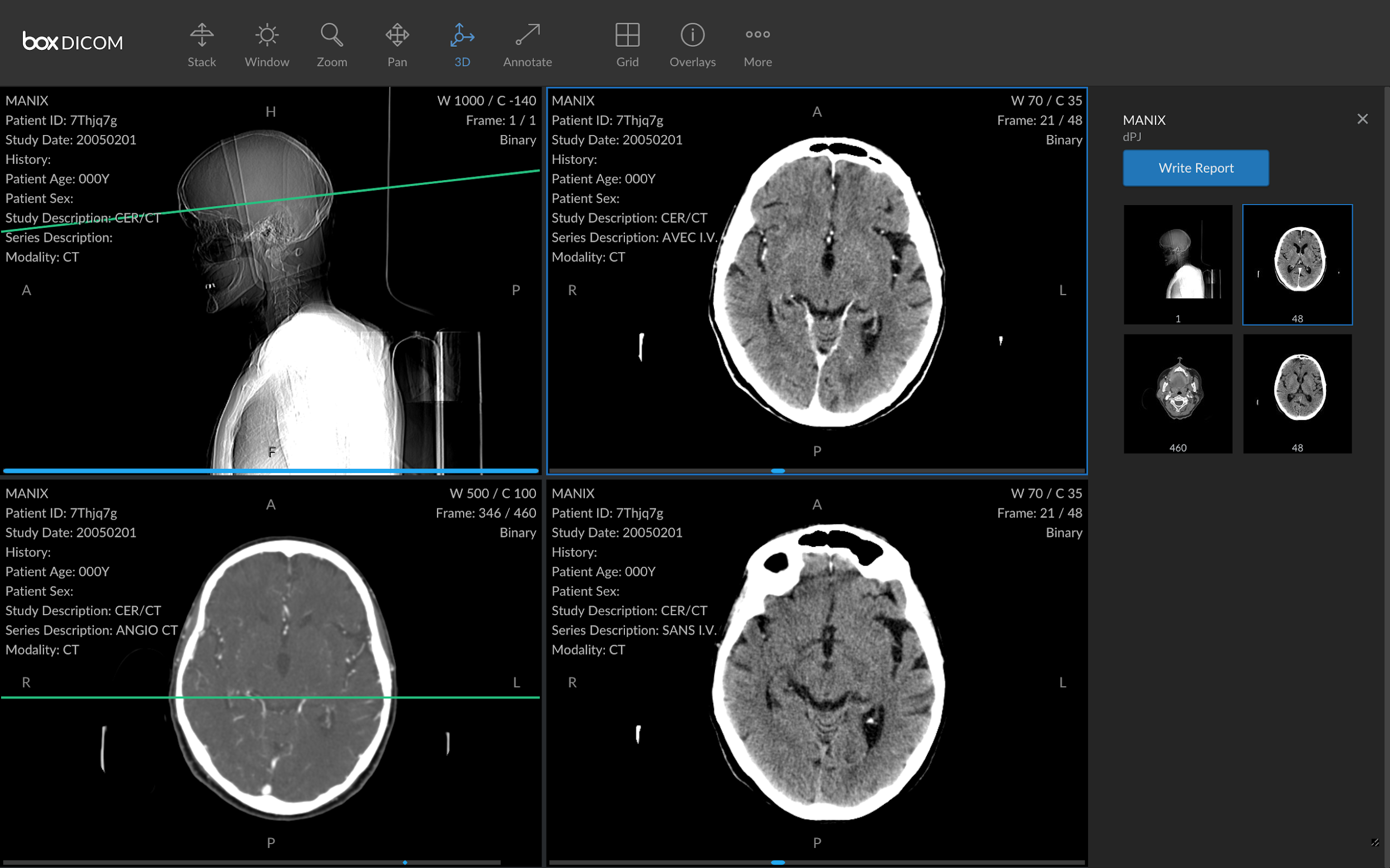
A DICOM file with images and metadata. Source: HIT Consultant
SCRIPT for electronic prescribing
The Script past NCPDP is an industry standard for exchanging electronic prescriptions and related information betwixt care providers, pharmacies, and health plans. Besides the submission of new prescriptions, it supports canceling and changing prescriptions, refilling requests, and other operations.
SCRIPT uses RxNorm codes for drug info and SNOMED codes for describing allergies. It also allows for adding a Continuity of Care Document attachment.
CDISC for medical research information exchange
Clinical Data Interchange Standards Consortium or CDISC standards are developed to improve the electronic exchange of clinical trial data between pharma companies and researchers. In 2016, the standards became mandatory for submitting trial information to regulatory authorities like the Food and Drug Administration (FDA).
To larn more than, read our dedicated article on CDISC Standards.
Privacy and security standards
Privacy and security standards establish authoritative and technical rules to protect sensitive wellness data from misuse, unauthorized admission, or disclosure.
HIPAA for health data beyond the The states
In the US, the privacy and security standards for medical information are outlined past the Health Insurance Portability and Accountability Act (HIPAA). Amongst other things, it formalizes the employ of ICD-10-CM, CPT, HCPCS, CDT, and NDC codes in medical billing.
HIPAA Privacy Dominion applies to individual medical records and other personal health data. It sets limits on the utilise and sharing of patient data for health plans, healthcare providers, and other players. The rule also empowers patients to freely access their medical records and request corrections to them.
HIPAA Security Dominion defines what electronic health information must exist protected and what technologies, policies, and procedures must be in place to ensure the appropriate level of security.
Our recent article explains how to reduce the run a risk of violating HIPAA rules.
In the European Wedlock, health information falls inside the scope of the General Data Protection Regulation (GDPR). To meet the standards, healthcare organizations must
- appoint a Data Protection Officer (DPO);
- conduct a Information Protection Impact Cess (DPIA) — or, in other words, evaluate data protection risks;
- implement a cybersecurity strategy; and
- report information breaches within 72 hours.
Similar to HIPAA standards, GDPR also gives patients the right to access their personal data.
Health data standards challenges and possible solutions to them
Obviously, the healthcare manufacture doesn't lack data standards. SDOs have developed plenty of them to comprehend nigh every aspect of advice between disparate health systems. But the mere fact of their being and availability doesn't tackle all the problems related to interoperability. Below we'll list some vexing challenges related to standards and potential ways to address them.
Medical coding speed and accuracy issues
Transformation of diagnoses, procedures, services, handling plans, and other concepts into medical codes involves a lot of manual work, performed by especially trained professionals. Today coders rely on figurer-assisted coding systems. However, the speed and accurateness of the translating procedure are far from perfect.
To that end, big hopes are pinned on AI-fueled software capable of identifying correct codes and suggesting them for experts to review. Currently, such intelligent systems make coding faster, however, they tin can't fully supervene upon humans and automate the unabridged process.
Demand for mapping betwixt codes
Each code in healthcare does its ain job: SNOMED enables physicians to draw a detailed clinical picture of a patient treated, ICD-10 briefly describes diagnoses, CPT summarizes services.
That said, there are situations when translation from one code arrangement to another is needed. For example, as nosotros mentioned earlier, SNOMED tin't be used for billing purposes and must be translated to ICD-10-CT.
Standard development organizations endeavor unlike options to accost mapping challenges. Say, SNOMED CT runs Mapping Project Group that is working on automatic methods of linking two terminologies.
Lack of compatibility betwixt former and new standards
To comply with existing interoperability rules, hospitals must ensure the availability of content defined by USCDI through FHIR-based APIs. Just permit's face up the truth: Most EHR systems were built with a view to old standards. Some of them can exercise no more than importing and exporting HL7 v2 messages. Others mainly rely on C-CDA documents.
Neither v2 nor C-CDA fits into granular USCDI information elements or FHIR basic exchangeable data blocks — resources. And then, hospitals need additional digital tools and human resources to excerpt data from older formats and convert them into FHIR and USCDI compatible elements. At that place are several initiatives to accost this trouble like the C-CDA on FHIR implementation guide or v2-to-FHIR project.
No two-way communication between patients and EHRs
FHIR standard allows patients to get health data via apps of their choice. However, this is a ane-manner street equally EHRs grant read-just access to their systems. A person can request information but take no means to command and alter it through the app.
Many industry experts argue that the lack of 2-style communication betwixt medical apps and EHR systems is the next biggest challenge for healthcare. And sooner or afterward, it will require creating new data standards.
How can stakeholders impact the situation and contribute to improve communication between all parties? The respond is to actively participate in standard development processes, submit feedback, and share their ideas with the standards customs.
Why Are Open Standards Important In The Data Communications Industry?,
Source: https://www.altexsoft.com/blog/data-standards-healthcare/
Posted by: fettermanfatabimpar1961.blogspot.com


0 Response to "Why Are Open Standards Important In The Data Communications Industry?"
Post a Comment